Cannabis and Surgery: What Every Surgeon and Anesthesiologist Should Know
My inspired takeaways from a meta-analysis discussed at a journal club
Cannabinoid exposure is on the rise, and with it comes a growing concern: how does pre-operative cannabinoid or cannabis/hemp use impact surgical outcomes? While patients often turn to cannabis for pain relief, a recent meta-analysis in Frontiers in Public Health suggests that a history of cannabis use may lead to increased complications after total hip (THA) and knee arthroplasty (TKA).
The systematic review analyzed data from 16 cohort studies involving nearly 6 million patients and found that cannabis use was associated with experiencing higher rates of prosthetic failure, cardiovascular complications, and infections. These findings challenge the common perception that cannabis is harmless in a surgical setting.
Does Cannabis Use Matter in Surgery?
Many cannabis users undergoing elective surgery don’t disclose their use to doctors—either because they don’t see it as relevant or because it’s not explicitly asked about in preoperative screening. As Ata Kiapour, PhD, MMSc, director of Boston Children’s Musculoskeletal Informatics Group, points out:
This lack of screening means that many anesthesiologists and surgeons are unknowingly treating cannabis users without adjusting their approach, despite evidence that cannabis may alter anesthesia requirements, pain perception, and post-surgical healing.
Key Findings: Increased Risks for Joint Replacement Patients
The meta-analysis identified significant risks associated with cannabis use in total joint replacement surgeries:
o Higher risk of revision surgery (RR 1.68)
o Increased implant failure (loosening, fractures, dislocation)
o Greater risk of cardiovascular and cerebrovascular complications (RR 2.49–3.15)
o Higher rates of pneumonia, UTIs, and respiratory failure
o Twice the likelihood of requiring a blood transfusion
o Higher hospitalization costs ($16,938–$59,570 for cannabis users vs. $16,023–$53,316 for non-users)
However, cannabis was not associated with any change in post-op opioid use or pulmonary embolism, suggesting that its effects may be more mechanical and immune-related rather than respiratory.
Bone Healing and Implant Failure: The Missing Piece?
One of the most concerning findings was the higher rate of periprosthetic fractures and implant failure in cannabis users. While the meta-analysis didn’t explore the underlying cause, other research suggests cannabis may impair bone healing.
In a 2021 study, orthopedic surgeon Grant Hogue, MD, analyzed urine toxicology screenings of adolescent trauma patients with extremity fractures. Based on that work Hogue speculated,
If cannabis delays healing in young patients, what does that mean for older adults undergoing joint replacement, where bone healing is already slower?
Does Cannabis Interact with Anesthesia?
As cannabis use grows, surgeons and anesthesiologists are calling for better patient disclosure and improved screening practices. According to Dr. Jennifer Kollman, anesthesiologist and senior medical director for anesthesia at UCHealth in Colorado:
Another major concern is cannabis-anesthesia interactions. Research suggests cannabis users may require higher doses of anesthetics and sedatives to achieve the same level of clinical anesthesia:
Some evidence suggests cannabis may enhance or prolong the effects of inhaled anesthetics like isoflurane and sevoflurane.
Conversely, cannabis may increase the need for GABAergic anesthetics such as propofol, midazolam, and benzodiazepines.
This variability makes dosing unpredictable, increasing the risk of delayed emergence from anesthesia or intraoperative awareness.
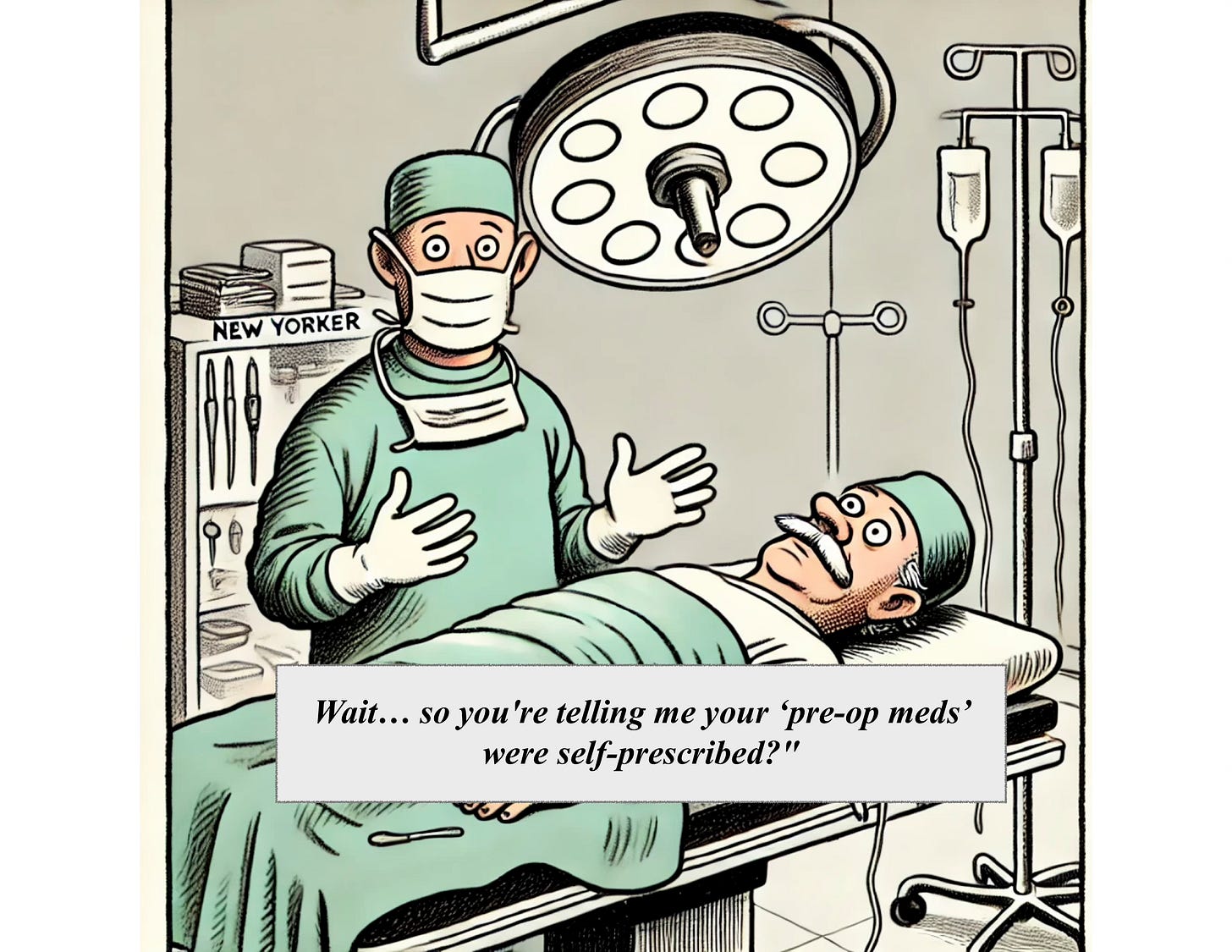
As one of the slides in the Cerium Journal Club presentation (insert link to youtube video) asks:
“If you were an anesthesiologist [or the surgeon], wouldn’t you want to know if the patient you’re about to put under was a cannabis user?”
How Should Surgeons and Anesthesiologists Respond?
With cannabis use increasing, it’s time for hospitals and surgical teams to adapt.
1. Improve Preoperative Screening
Include cannabis use questions in patient intake forms alongside tobacco and alcohol.
Differentiate between occasional vs. chronic cannabis use to better assess risk.
2. Adjust Anesthesia and Pain Management Plans
Be aware that cannabis users may require different dosing strategies for anesthesia.
Consider non-opioid pain management options, as cannabis users may have altered pain perception.
3. Educate Patients on the Risks
Patients need to understand that cannabis may not be risk-free in surgery—it may affect healing, increase complications, and prolong recovery.
Encourage preoperative cannabis cessation to optimize surgical outcomes.
4. Continue Research into Cannabis-Surgical Interactions
There will never be randomized clinical trials on cannabis and elective surgeries, but more observational data is needed.
Future research should explore dose-response relationships, long-term outcomes, and cannabis use disorder in surgical patients.
The Bottom Line
The idea that cannabis is “just a plant” and has no impact on surgery is outdated. As more research emerges, it’s becoming clear that cannabis use—particularly chronic use—should be factored into preoperative planning. Surgeons and anesthesiologists need to ask the right questions, adjust protocols, and educate patients about these risks. Patients should be encouraged to disclose their cannabis use honestly and consider reducing or pausing use before surgery.
For now, the best approach is caution and awareness. The risks are real—so the next time a patient comes in for an elective procedure, will their cannabis use be part of the conversation?
What do you think? Should hospitals implement routine cannabis screening before joint replacements? Share your thoughts.